In physiotherapy, the ultimate goal is to restore function, improve strength, mobility, and range of motion, and minimize pain for individuals recovering from injury or surgery. A critical part of achieving this involves the use of specific exercise techniques, particularly open and closed kinematic chain exercises. These exercises form the backbone of rehabilitation programs, helping patients progress safely and effectively toward full recovery.
This blog will explore what these exercises entail, their respective advantages, and how they are used in physiotherapy treatment.
Understanding Kinematic Chains: Open vs. Closed
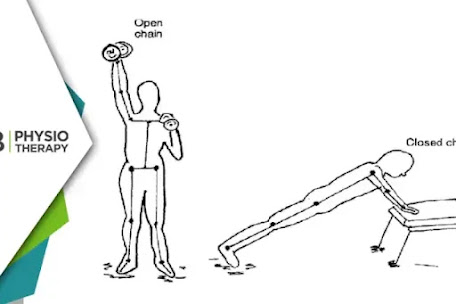
Kinematic chain exercises refer to movements that involve multiple joints and muscles working together in a sequence. These exercises are broadly categorized into two types: open and closed kinematic (or kinetic) chain exercises.
Open Kinematic Chain Exercises In an open kinematic chain (OKC) exercise, the distal (farthest) part of the limb moves freely in space, without a fixed point of contact with the surface. For example, when you kick a ball or extend your leg while seated, the foot (distal limb) is free to move, and the rest of the body remains relatively stationary. OKC exercises typically isolate a specific muscle group or joint, focusing on improving strength and range of motion in a controlled and targeted manner.
Examples of Open Kinematic Chain Exercises:
1. Leg extensions
2. Bicep curls
3. Seated knee extensions
4. Shoulder presses
Closed Kinematic Chain Exercises In contrast, closed kinematic chain (CKC) exercises involve movements where the distal limb is fixed or in contact with a surface (ground or another stable object), and the body moves in relation to it. For example, during a squat, the feet remain in contact with the ground while the body moves. CKC exercises tend to engage multiple muscle groups simultaneously, promoting joint stability and overall coordination.
Examples of Closed Kinematic Chain Exercises:
1. Squats
2. Push-ups
3. Lunges
4. Deadlifts
Role of Open and Closed Kinematic Chain Exercises in Physiotherapy
Both open and closed chain exercises have distinct roles in rehabilitation, offering unique benefits depending on the patient’s needs and the specific phase of treatment. The decision to incorporate either or both types depends on factors such as the type of injury, the joint involved, the stage of healing, and the goals of therapy.
1. Open Kinematic Chain Exercises: Targeted Strengthening and Range of Motion OKC exercises are ideal for isolating and strengthening specific muscles or joints. In the early stages of rehabilitation, particularly following surgery or injury, physiotherapists often prioritize OKC exercises because they place less overall stress on the joints, reducing the risk of re-injury while allowing controlled muscle activation.
a: Advantages of Open Kinematic Chain Exercises:
1. Isolation of Specific Muscles: OKC exercises are excellent for targeting individual muscles that may be weak or underused due to injury. For example, after ACL reconstruction surgery, physiotherapists may prescribe knee extensions to target the quadriceps.
2. Improved Range of Motion: These exercises are beneficial for improving the range of motion in joints like the knee or shoulder. Isolated movements help stretch and strengthen muscles around the joint, facilitating recovery of movement patterns.
3. Early-Stage Rehabilitation: OKC exercises are often used in the early stages of treatment when the patient may not yet be able to tolerate weight-bearing activities. They allow for muscle activation without placing undue strain on healing tissues.
b: Clinical Application of Open Kinematic Chain Exercises:
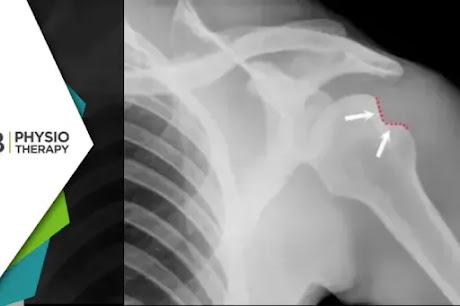
1. Post-Surgery Rehabilitation: After surgeries like a knee replacement or rotator cuff repair, OKC exercises are often prescribed to gradually strengthen muscles without stressing the joint.
2. Rehabilitation of Non-Weight Bearing Injuries: OKC exercises are critical in scenarios where weight-bearing is not advised, such as in certain fractures or post-operative conditions.
2. Closed Kinematic Chain Exercises: Functional Strength and Joint Stability CKC exercises are more functional in nature and closely mimic the movements that patients perform in their daily activities. These exercises recruit multiple muscle groups, promoting coordination, balance, and joint stability. In physiotherapy, CKC exercises are particularly beneficial for improving proprioception (awareness of joint position), which is often impaired after injury.
A: Advantages of Closed Kinematic Chain Exercises:
1: Joint Stability: CKC exercises help stabilize joints by engaging multiple muscles around the joint. For example, during a squat, the quads, hamstrings, and glutes all work together to provide stability to the knee joint, reducing the risk of injury.
2: Functional Movement Patterns: These exercises mimic everyday movements, making them highly functional. For example, squats and lunges resemble activities like standing up from a chair or climbing stairs, helping patients regain the ability to perform daily tasks.
3: Improved Proprioception: Because CKC exercises involve weight-bearing movements, they are excellent for enhancing proprioception and balance. This is particularly important for patients recovering from lower extremity injuries, such as ankle sprains or knee ligament tears.
4: Multi-Joint Coordination: CKC exercises engage multiple joints and muscle groups simultaneously, improving coordination and helping patients restore full-body strength and stability.
B: Clinical Application of Closed Kinematic Chain Exercises:
1: Late-Stage Rehabilitation: As patients progress through their rehabilitation program, CKC exercises are introduced to improve functional strength and prepare them for the demands of daily life or sports activities. For example, after knee surgery, physiotherapists may prescribe squats and lunges to strengthen the lower limbs and improve overall stability.
2: Prevention of Re-Injury: CKC exercises are crucial for preventing future injuries by reinforcing joint stability and muscle coordination. This is particularly beneficial for athletes returning to sports after injury.
Combining Open and Closed Kinematic Chain Exercises in Physiotherapy
For optimal results in physiotherapy, combining both OKC and CKC exercises is often the most effective approach. The integration of these exercises allows for comprehensive rehabilitation, addressing both the specific muscle weakness and the overall functional stability of the body.
1: Early-Stage Rehabilitation:
In the initial phases of rehabilitation, OKC exercises are typically prioritized to isolate and strengthen specific muscles. For example, after an ACL reconstruction, the physiotherapist may focus on leg extensions to target the quadriceps without placing too much stress on the healing knee joint.
2: Mid-to-Late Stage Rehabilitation:
As the patient progresses, CKC exercises like squats and lunges are introduced to promote joint stability, functional strength, and proprioception. This prepares the patient for the demands of everyday activities and sports, ensuring that the joint can handle complex, multi-joint movements.
By incorporating both open and closed chain exercises, physiotherapists can tailor rehabilitation programs to meet the individual needs of each patient, ensuring a safe and effective recovery. Understanding the importance and proper application of these exercises allows patients to regain strength, mobility, and function more effectively, ultimately improving their quality of life.