The shoulder joint, being one of the most mobile joints in the human body, is vulnerable to dislocation and associated injuries. One of the common complications of shoulder dislocation is a Hill-Sachs lesion-a compression fracture or indentation on the posterolateral aspect of the humeral head. This lesion is often associated with recurrent shoulder dislocations, particularly in active or younger individuals. Understanding the biomechanics of this condition and how physiotherapy can manage it is crucial for effective rehabilitation and prevention of further dislocations.
Understanding a Hill-Sachs Lesion
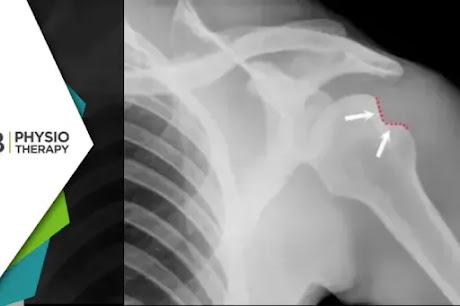
A Hill-Sachs lesion occurs when the humeral head, the ball of the shoulder joint, forcefully impacts the edge of the glenoid cavity (socket) during a shoulder dislocation. The most common type of shoulder dislocation is anterior dislocation, where the humeral head slips out of the socket in a forward direction. As the humeral head is driven against the glenoid rim, it creates a dent or compression fracture on the humerus, which is referred to as a Hill-Sachs lesion.
Link Between Hill-Sachs Lesion and Recurrent Shoulder Dislocation
When a Hill-Sachs lesion is present, it alters the shape of the humeral head, making it more prone to catching on the rim of the glenoid, particularly during movements that involve external rotation and abduction (raising the arm sideways). This biomechanical alteration increases the risk of the shoulder slipping out of place again, resulting in chronic shoulder instability.
In more severe cases, a Bankart lesion-damage to the anterior labrum of the shoulder-may accompany the Hill-Sachs lesion, further destabilizing the joint. The combination of these injuries can lead to recurrent shoulder dislocations, especially in athletes who participate in contact sports or individuals who frequently engage in overhead activities.
The symptoms of a Hill-Sachs lesion may vary depending on its severity and the frequency of shoulder dislocations. Common signs include shoulder pain that worsens with movement, sense of instability or weakness in the shoulder, particularly during overhead movements, limited range of motion, especially in external rotation and abduction, recurrent dislocations, sometimes with minimal force, creaking or clicking sounds during shoulder movements. If left untreated, these symptoms can progressively worsen, significantly impacting a person’s daily life and activities.
Physiotherapy in the Management of Hill-Sachs Lesion and Shoulder Instability Physiotherapy plays a pivotal role in managing both the immediate and long-term effects of a Hill-Sachs lesion, particularly in preventing recurrent shoulder dislocations. The primary goals of physiotherapy are to:
1: Restore shoulder strength and stability.
2: Improve joint proprioception.
3: Enhance functional movement patterns.
4: Reduce the risk of future dislocations.
1. Initial Phase: Pain and Inflammation Management
Following a shoulder dislocation and diagnosis of a Hill-Sachs lesion, the initial focus of physiotherapy is to control pain and inflammation. Modalities such as ice therapy, electrical stimulation, and manual therapy may be used to manage pain and promote healing of the injured tissues. Immobilization of the shoulder in a sling may be recommended for a short period, but prolonged immobilization should be avoided to prevent stiffness and muscle weakness.
2. Restoring Range of Motion (ROM)
Once pain and inflammation are under control, the next phase involves gradually restoring range of motion in the shoulder joint. This is done through passive and active-assisted exercises that focus on gently stretching the muscles and soft tissues surrounding the shoulder. Some examples of ROM exercises include:
1: Pendulum exercises: These involve gently swinging the arm in a circular motion while leaning forward, which helps increase joint mobility without putting stress on the shoulder.
2: Passive shoulder flexion and external rotation: The therapist may assist the patient in gently raising the arm overhead or rotating the arm outward.
It’s crucial to avoid any activities that place excessive strain on the shoulder, such as lifting heavy objects or performing sudden overhead movements, as this could lead to further dislocation.
3. Strengthening Shoulder Muscles
Once full or near-full range of motion is achieved, the focus shifts to strengthening the muscles that support and stabilize the shoulder joint. The rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) play a critical role in maintaining shoulder stability and preventing dislocations.
Strengthening exercises should be progressive and target both the rotator cuff and scapular stabilizers to ensure proper shoulder mechanics. Some effective strengthening exercises include:
1: Isometric shoulder exercises: These involve contracting the shoulder muscles without moving the joint, helping to build strength without aggravating the lesion.
2: External and internal rotation exercises: Using resistance bands or light weights, patients can gradually build strength in the rotator cuff muscles, particularly the infraspinatus and subscapularis.
3: Scapular stabilization exercises: Strengthening the muscles around the scapula (shoulder blade) is important for overall shoulder stability. Exercises such as scapular retractions and wall push-ups can be helpful.
4. Enhancing Proprioception and Neuromuscular Control
Proprioception refers to the body’s ability to sense its position in space. In the case of shoulder instability, proprioception is often impaired, making it difficult for the body to detect when the shoulder is in a vulnerable position. Physiotherapy aims to improve proprioception through exercises that enhance neuromuscular control.
Balance and coordination exercises, such as using a stability ball, wobble board, or performing closed-chain exercises like weight-bearing shoulder taps, can help improve proprioception and prevent further dislocations.
5. Functional Training and Return to Activity
As strength and stability improve, the final phase of physiotherapy involves functional training that mimics the patient’s daily activities or sports-related movements. The goal is to ensure that the shoulder can safely handle the demands of daily life or athletic performance without the risk of re-injury.
In cases of severe Hill-Sachs lesions or when recurrent dislocations persist despite comprehensive physiotherapy, surgical intervention may be considered. lesions. In such cases physiotherapy is essential post-surgery to ensure a successful recovery and prevent future instability.